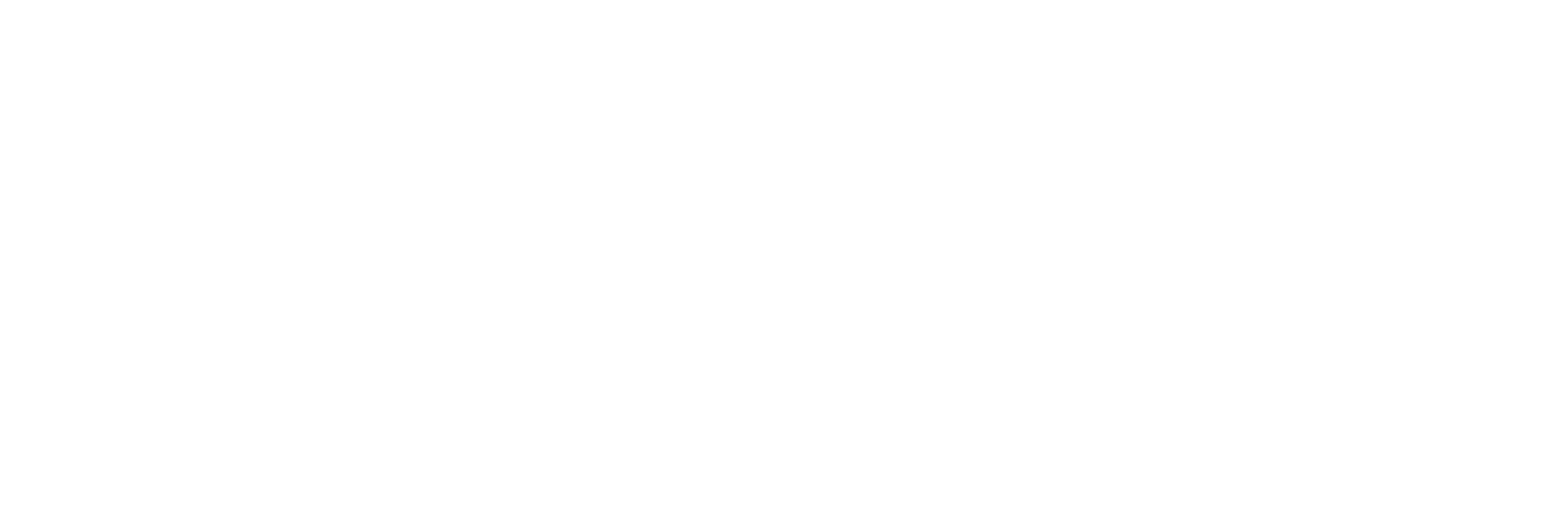
In the ongoing battle against opioid addiction, a groundbreaking prediction model has emerged, offering a beacon of hope for individuals grappling with opioid use disorder (OUD). This advanced tool stands to transform the landscape of addiction treatment by providing an early warning system for relapse risk, thereby enabling timely and tailored intervention strategies.
- Understanding the Prediction Model’s Mechanics
- The Role of Medications in Opioid Use Disorder
- Risk Scores: A Novelty in Opioid Treatment
- Harnessing Machine Learning for Precision
- The Power of Early Detection
- Implications for Treatment Strategies
- The Road Ahead: Clinical Trials and Long-term Data
- A Call to Action for Clinicians and Researchers
- Conclusion
Understanding the Prediction Model’s Mechanics
At the core of this innovation is a prediction model meticulously crafted using a robust dataset from 2,199 adults participating in clinical trials for opioid medication treatments. Its predictive prowess lies in its ability to gauge the likelihood of a patient’s return to opioid use within the initial 12-week treatment regimen.
This model isn’t just a theoretical concept; it is a practical tool made accessible through a dedicated web portal (www.oudriskscore.org) designed for clinicians to calculate their patients’ relapse risks swiftly. Such a tool is pivotal in customizing treatment plans, especially for those at heightened risk of relapse, and is a significant step forward in personalized medicine.
The Role of Medications in Opioid Use Disorder
Medications like methadone, buprenorphine, and extended-release injection naltrexone have long been the cornerstone of OUD treatment. However, their efficacy is not absolute, and relapse during treatment is a persistent challenge. The prediction model brings a nuanced understanding of how treatment dosages and forms might be optimized for individual patients, such as considering increasing buprenorphine doses or transitioning to extended-release injections for better outcomes.
Risk Scores: A Novelty in Opioid Treatment
In treating chronic illnesses, risk scores are commonplace to forecast health events and inform treatment decisions. However, this method is novel in the context of OUD treatment. The model developed offers clinicians a way to anticipate relapse risks, paving the way for proactive adjustments to treatment plans.
Harnessing Machine Learning for Precision
The model’s development employed machine learning techniques to distill vast clinical trial data Information in analog or digital form that can be transmitted or processed. Read Full Definition into a predictive tool. Utilizing the LASSO method, the model identifies and integrates key patient characteristics to forecast relapse probability. This approach ensures that the model remains both comprehensive and precise"Precise" refers to the degree of closeness or consistency between multiple measurements or values taken under the same conditions. It indicates how well these measurements agree with each other, regardless of whether they are accurate Read Full Definition, leveraging the full scope of available data to support patient care.
Information in analog or digital form that can be transmitted or processed. Read Full Definition into a predictive tool. Utilizing the LASSO method, the model identifies and integrates key patient characteristics to forecast relapse probability. This approach ensures that the model remains both comprehensive and precise"Precise" refers to the degree of closeness or consistency between multiple measurements or values taken under the same conditions. It indicates how well these measurements agree with each other, regardless of whether they are accurate Read Full Definition, leveraging the full scope of available data to support patient care.
The Power of Early Detection
One of the model’s standout features is its capacityThe amount of finished product that could be produced, either in one batch or over a defined period of time, and given a set list of variables. Read Full Definition to incorporate early treatment data, such as urine drug test results, to refine risk predictions. Patients who have negative or no missed drug tests in the initial weeks of treatment are shown to have a significantly lower risk of relapse. This vital insight allows for more nuanced patient monitoring and can be the difference between a successful recovery and a return to use.
Implications for Treatment Strategies
The utility of this model extends beyond risk assessment; it serves as a guide for actionable strategies. For patients flagged as high-risk, the model suggests intensified monitoring, dose adjustments, and the integration of psychotherapeutic support. These recommendations are not mere suggestions but are grounded in empirical evidence
The Road Ahead: Clinical Trials and Long-term Data
The call for new clinical trials is clear as we seek to refine treatment strategies for those at high risk of relapse. Furthermore, extending the follow-up period beyond the initial 12-week phase is crucial for understanding the long-term patterns of opioid use and relapse, thereby enhancing the model’s predictive accuracyIn scientific and measurement contexts, "accuracy" refers to the degree of proximity or closeness between a measured value and the true or actual value of the measured quantity. Accuracy indicates how well a measurement reflects Read Full Definition and reliability.
A Call to Action for Clinicians and Researchers
As the model continues to demonstrate its value, it is incumbent upon the medical community to embrace this tool, integrate it into practice, and contribute to its ongoing refinement. Researchers are also encouraged to explore the model’s applications and continuously seek new data sources to enhance its predictive capabilities.
Conclusion
The introduction of this prediction model signifies a significant advancement in the treatment of opioid use disorder. It embodies the convergence of clinical expertise, data analytics, and machine learning to offer a real-world solution that can save lives. By providing clinicians with the ability to anticipate and preempt relapse, we are one step closer to turning the tide on the opioid epidemic.