Did you know that traditional autopsies face significant limitations when cultural or religious beliefs restrict post-mortem examinations? Virtual autopsy offers a solution through non-invasive digital technology, employing advanced CT scanning to create detailed 3D models of the body’s interior. This technique allows forensic pathologists to examine remains without disturbing bodily integrity, marking a significant step forward in death investigations.
- What is a Virtual Autopsy: Definition and Core Technologies
- Origins of Digital Post-Mortem Analysis
- Technologies involved
- CT Scanning in Post-Mortem Examination
- MRI Applications for Soft Tissue Analysis
- 3D Surface Scanning and Reconstruction
- The Virtual Autopsy Process: Step-by-Step Workflow
- Initial Body Documentation and External Examination
- Internal Scanning Protocols
- Data Processing and 3D Reconstruction
- Virtual Dissection Techniques
- Benefits of Virtual Autopsy
- A. Non-invasive procedure
- B. Faster results
- C. Preservation of evidence
- D. Cultural and religious considerations
- Advanced Imaging Technologies in Virtual Autopsy
- Post-Mortem Angiography for Vascular Visualization
- Magnetic Resonance Spectroscopy for Time of Death Estimation
- Microtomography for Microscopic Injury Analysis
- Forensic Applications of Virtual Autopsy
- Trauma Pattern Analysis and Weapon Identification
- Foreign Object Detection and Localization
- Cause of Death Determination Accuracy
- Disaster Victim Identification Protocols
- Comparing Virtual Autopsy to Traditional Methods
- Diagnostic Accuracy Rates in Different Scenarios
- Time and Resource Requirements
- Preservation of Evidence
- Limitations in Physiological Assessment
- Comparison with traditional autopsy
- Technical Challenges and Scientific Limitations
- Current Hardware Constraints
- Software Development Needs
- Data storage and security
- Legal and ethical considerations
- Standardization of Protocols
- Training Requirements for Forensic Radiologists
- Future of Virtual Autopsy
- Conclusion
- FAQs
- What are the main advantages of virtual autopsy over traditional methods?
- How accurate is virtual autopsy in determining the cause of death?
- What technologies are used in virtual autopsy?
- Can virtual autopsy completely replace traditional autopsy methods?
- What are the main challenges in implementing virtual autopsy systems?
The technology behind virtual autopsies relies on specialized software systems like VizOpsy™. These platforms enable forensic experts to conduct thorough post-mortem examinations through precise"Precise" refers to the degree of closeness or consistency between multiple measurements or values taken under the same conditions. It indicates how well these measurements agree with each other, regardless of whether they are accurate Read Full Definition 3D volume analysis and detailed visualization of internal structures. Studies from the University of Bern’s Institute of Forensic Medicine demonstrate this approach’s effectiveness, with findings showing the technology successfully identified 55% of causes of death that conventional autopsies discovered.
We’ll examine how virtual autopsyAn autopsy, also known as a post-mortem examination or necropsy (when performed on animals), is a thorough and systematic medical procedure that involves the examination of a deceased person's body, typically to determine or confirm Read Full Definition works, from basic scanning principles to advanced reconstruction techniques. The process combines multiple imaging modalities to create comprehensive digital models that forensic experts can manipulate and analyze. This non-invasive method preserves evidence
What is a Virtual Autopsy: Definition and Core Technologies
Virtual autopsy, also known as digital autopsy or virtopsy, is a non-invasive post-mortem examination technique that utilizes advanced medical imaging technologies to investigate the cause of deathThe cause of death refers to the specific injury, disease, or underlying condition that directly leads to an individual's demise. It is a critical determination made by medical professionals, such as Medical Examiners or Coroners, Read Full Definition. This innovative approach combines high-resolution CT scans, MRI, and 3D reconstruction to create detailed digital models of the deceased, allowing forensic experts to examine the body without the need for physical dissection.

A virtual autopsy represents a significant departure from traditional post-mortem examinations. This method uses advanced imaging technologies to investigate a body’s internal structures without making physical incisions. The approach preserves bodily integrity while creating detailed digital visualizations for forensic analysis. Interestingly, the term “Virtopsy”—a blend of “virtual” and “autopsy”—is a registered trademark of Richard Dirnhofer, former head of the Institute of Forensic Medicine at the University of Bern, Switzerland.
Origins of Digital Post-Mortem Analysis
The roots of digital post-mortem analysis can be traced to the late 1990s, when the Virtopsy® research project launched in Switzerland. This groundbreaking initiative initially combined results from conventional autopsies with forensic imaging using CT, MRI, and 3D surface scanning. The primary goal was straightforward yet ambitious: to detect forensic findings in corpses using radiological methods and compare these with traditional autopsy results.
As research progressed, the Virtopsy® project expanded its methodology. The team incorporated additional techniques, such as post-mortem biopsy and angiography, to enhance its investigative capabilities. Under the leadership of Professor Michael Thali at the Institute of Forensic Medicine in Zurich, who co-founded the project in 1999, virtual autopsies have become the standard procedure in Switzerland.
Meanwhile, Japan developed a parallel approach called “Autopsy imaging” (locally abbreviated as “Ai”) around 2000. The technique gained significant traction there, with a 2021 report indicating that 34.5% of unusual death cases (17,0174 out of 58,689 cases) underwent postmortem CT scanning in 2018.
Technologies involved
The virtual autopsy process employs a combination of cutting-edge imaging technologies:
- Computed Tomography (CT) scanning
- Magnetic Resonance Imaging (MRI)
- 3D surface scanning
- Advanced visualization software
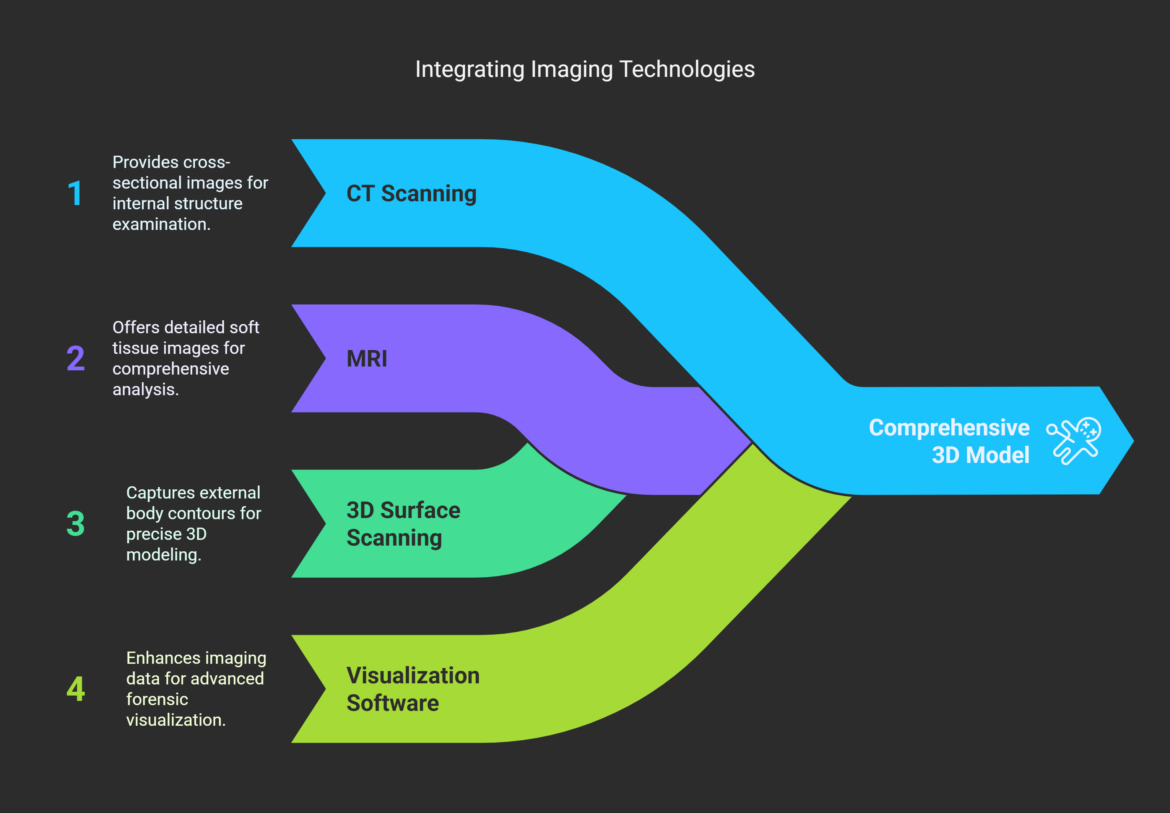
These technologies work together to create a comprehensive 3D model of the body, allowing forensic experts to examine internal structures with remarkable detail and precision. Integrating these imaging methods provides a powerful tool for forensic investigations and medical research.
CT Scanning in Post-Mortem Examination
Computed tomography, aside from standard X-rays, is the most commonly used imaging tool in forensic pathology. Today’s CT scanners produce remarkably detailed 2D and 3D reconstructions based on slice thicknesses of just 0.5 mm. During standard PMCT (Post-Mortem Computed Tomography) procedures, the body is positioned supine, with the upper extremities in a natural drooping position.
CT scanning provides four key advantages in post-mortem examination:
- Superior visualization of skeletal traumatic lesions, foreign bodies, gas, and fluid accumulations
- Comprehensive coverage from head to pelvis during scanning
- Preservation of evidence, as medical devices such as catheters and tubes can remain in place during imaging
- Efficient processing with the ability to take up to 3,500 x-ray slices from head to toe
The impact of PMCT on forensic investigations has been substantial. One study found that this technology affected the final determination of cause and manner of death in 20% of cases. In New Mexico, the Office of the Medical Investigator decreased complete autopsies by 10% over five years (2013-2018) after implementing post-mortem CT scanning, despite handling 15% more cases overall.
MRI Applications for Soft Tissue Analysis
While CT excels at bone and foreign object detection, Magnetic Resonance Imaging (MRI) offers superior soft-tissue visualization. PMMR (Post-Mortem Magnetic Resonance) provides exceptional anatomical detail for examining pathologies of the brain, heart, subcutaneous fat tissue, and abdominal organs.
T2-weighted MR images are crucial in post-mortem imaging because they effectively highlight fluid accumulations. This capability makes them ideal for diagnosing conditions like subcutaneous hematoma, bone contusion, organ laceration, internal hemorrhage, ischemic heart injury, and brain edema. STIR sequences have proven particularly valuable for screening purposes, as they emphasize signals from tissues with long T2 relaxation times. This causes fluid accumulations to “flash like light bulbs” when reviewing image sequences.
Cardiovascular examination has consequently emerged as a core application for PMMR. Growing evidence suggests that PMMR can detect ischemic injury earlier than conventional autopsy and routine histology.
3D Surface Scanning and Reconstruction
Surface documentation forms another critical component of virtual autopsies. This process typically employs structured light scanning, where a fringe pattern is projected onto the body’s surface and recorded by dual cameras. Specialized software then calculates a 3D image from this data Information in analog or digital form that can be transmitted or processed. Read Full Definition.
Information in analog or digital form that can be transmitted or processed. Read Full Definition.
For example, the ATOS Compact Scan 5 system consists of a projector and two cameras that determine 3D topology by analyzing how the projected pattern distorts as it moves across the body during scanning. Technicians can achieve true color 3D surface reconstruction by integrating digital photography from multiple angles.
This highly precise documentation—capable of recording structures smaller than 1 mm depending on resolution settings—extends beyond body examination. It can document vehicles and injury-causing instruments and even match evidence like shoe imprints to injuries on a victim’s body. In one notable case, investigators used 3D photogrammetry and surface scanning to match several perpetrators’ shoes to imprints discovered on a victim’s face, arms, and armpit.
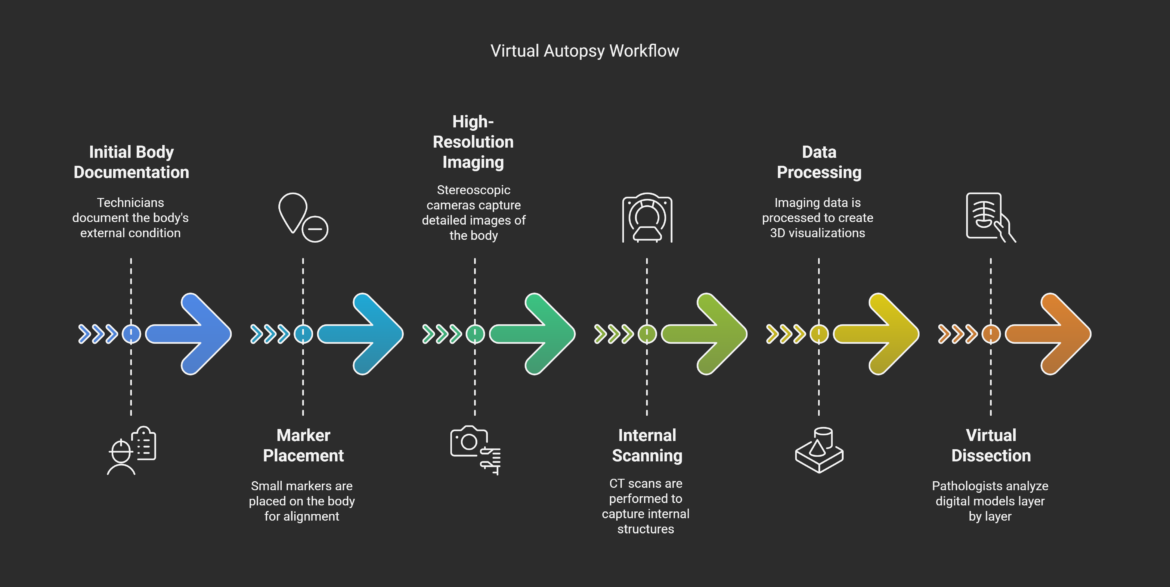
The Virtual Autopsy Process: Step-by-Step Workflow

Virtual autopsy follows a systematic workflow that prioritizes evidence preservation while maximizing information collection. Unlike traditional methods, this approach integrates multiple imaging technologies to create a comprehensive digital record of post-mortem findings. The process combines external documentation with internal scanning to build complete 3D models for forensic analysis.
Initial Body Documentation and External Examination
Before internal examination begins, forensic technicians must thoroughly document the body’s external condition. This critical first step includes collecting circumstantial data and external findings that guide the radiologist’s approach to whole-body examination. Without this foundation, subsequent imaging could miss crucial details.
How do technicians ensure accurate alignment between external and internal data? Small marker disks are strategically placed along the body’s surface. Advanced facilities employ the Virtobot system, which automatically positions these markers, eliminating human inconsistencies and standardizing results.
Following marker placement, stereoscopic cameras capture high-resolution images (typically 0.02mm resolution) to create a detailed 3D color model of the body. Simultaneously, a mesh pattern projected onto the body’s surface captures topographical details. This meticulous approach produces objective, reproducible documentation of external findings that remains available for future reference.
Internal Scanning Protocols
After completing external documentation, the team proceeds to internal imaging. Timing matters significantly here—PMCT scans ideally occur within 48 hours of death to minimize decomposition artifacts. Throughout this process, the body remains in a specialized bag that allows X-ray penetration while maintaining hygiene standards.
Modern CT scanning is remarkably efficient. A typical whole-body scan finishes in approximately 20 seconds and generates up to 25,000 individual slice images. These high-resolution images form the foundation for all subsequent analysis.
Initial findings often determine whether additional specialized scans are needed. The radiologist may recommend PMCTA for vascular visualization or targeted MRI for specific soft tissue analysis [9]. This collaborative approach continues as the radiologist provides the forensic pathologist with a preliminary report to guide decisions about further procedures.
Data Processing and 3D Reconstruction
The real magic happens when powerful computing systems process the collected imaging data. In as little as 10 minutes, software can transform thousands of X-ray slices into crisp 3D visualizations. These reconstructions allow forensic pathologists to examine the body’s interior without physical dissection.
Different tissues absorb X-rays at varying levels, creating natural contrast that software enhances through standardized color schemes. Typically, air pockets appear blue, soft tissues beige, blood vessels red, and bones white. This intuitive color coding helps examiners quickly identify structures and abnormalities.
Forensic teams face the challenge of integrating various data formats for complex cases requiring multiple imaging approaches. Research groups like VIRTOPSY have developed methods for simultaneous image acquisition across multiple modalities. Alternatively, teams can apply step-by-step procedures for combining 3D data collected at different times.
Virtual Dissection Techniques
The final workflow phase involves virtual dissection, where examiners analyze digital models layer by layer. Unlike conventional autopsy, pathologists can “peel” through tissues with simple mouse clicks, enabling instant, flexible examination from multiple angles. This non-destructive approach preserves evidence while providing comprehensive visualization.
Modern facilities utilize sophisticated equipment like the Anatomy Table, which offers advanced tools for virtual dissection. These systems create immersive learning environments where students and professionals can interact with anatomical structures in real time.
When tissue samples become necessary, CT-guided needle biopsies provide a minimally invasive solution. Technicians can perform these procedures with remarkable precision using either a step-and-shot approach (verifying needle position after each movement) or CT fluoroscopy for real-time guidance. The most advanced facilities employ computer-assisted navigation with trackable probes for maximum accuracyIn scientific and measurement contexts, "accuracy" refers to the degree of proximity or closeness between a measured value and the true or actual value of the measured quantity. Accuracy indicates how well a measurement reflects Read Full Definition.
This systematic workflow transforms forensic examination into a data-rich, non-destructive process. Virtual autopsy sets new standards for thorough post-mortem analysis by preserving evidence integrity while enhancing visualization capabilities.
Benefits of Virtual Autopsy
A. Non-invasive procedure
Virtual autopsy, also known as digital autopsy, offers a revolutionary approach to post-mortem examinations. Unlike traditional autopsies, virtual autopsies are completely non-invasive, utilizing advanced imaging technologies such as CT scans and MRI to examine the body internally without the need for physical incisions.
This non-invasive nature brings several advantages:
- Preservation of body integrity
- Reduced risk of infection for medical personnel
- Ability to re-examine findings without additional procedures
- Enhanced visualization of internal structures
| Traditional Autopsy | Virtual Autopsy |
|---|---|
| Invasive procedure | Non-invasive |
| Physical incisions | Digital imaging |
| Limited re-examination | Unlimited re-examination |
| Potential infection risk | Minimal infection risk |
B. Faster results
Virtual autopsies significantly reduce the time required to obtain crucial forensic information. The speed of digital imaging and analysis allows for:
- Rapid data acquisition (typically within hours)
- Quick preliminary findings
- Faster identification of the cause of death in many cases
- Reduced backlog in forensic departments
C. Preservation of evidence
One of the key benefits of virtual autopsy is its ability to preserve evidence indefinitely. This is particularly crucial in forensic investigations and legal proceedings. Virtual autopsies offer:
- Digital archiving of all findings
- 3D reconstructions for future analysis
- Preservation of fragile evidence that might be destroyed in traditional autopsies
- Ability to share findings easily with other experts
D. Cultural and religious considerations
Virtual autopsies provide a culturally sensitive alternative to traditional post-mortem examinations. This is particularly important for:
- Religious groups that prohibit body alteration after death
- Families who wish to avoid invasive procedures on their loved ones
- Cases where cultural beliefs conflict with legal requirements for autopsy
By offering a non-invasive option, virtual autopsies help balance the needs of forensic investigation with respect for cultural and religious practices. This approach can lead to increased cooperation in sensitive cases and broader acceptance of post-mortem examinations in diverse communities.
Advanced Imaging Technologies in Virtual Autopsy
While standard imaging forms the foundation of virtual autopsy, several specialized technologies have dramatically expanded what we can observe in post-mortem examinations. These advanced imaging techniques allow forensic scientists to visualize structures and processes that would remain hidden even during conventional autopsies. These methods are particularly valuable because they provide crucial findings while maintaining the non-invasive nature that defines virtual autopsy.

Post-Mortem Angiography for Vascular Visualization
How do forensic pathologists examine blood vessels in deceased individuals? Post-mortem angiography offers a solution by introducing contrast agents into the vascular system, revealing detailed images of blood vessels that would be difficult to assess through other means.
The most common technique involves a roller pump that administers an ionized water-soluble contrast medium combined with polyethylene glycol throughout the body’s circulatory system. This approach essentially mimics blood circulation in the deceased by creating artificial perfusion. Unlike clinical angiography performed on living patients, the absence of natural circulation requires mechanical injection to ensure both arterial and venous vessels receive adequate contrast.
The effectiveness of PMCTA (Post-Mortem CT Angiography) has been clearly demonstrated through research. Studies show it can identify an impressive 94% of vascular lesions, compared to just 65% detection rate with conventional autopsy methods. This capability proves especially valuable in traumatic death investigations, where PMCTA excels at visualizing the combined bone and vascular injuries typically seen in falls, traffic accidents, and gunshot wounds.
Perhaps most significantly, this technique visualizes vascular pathologies in regions not routinely examined during standard autopsies, including the craniocervical junction and small pelvis. By preserving essential evidence that might otherwise be disturbed or destroyed during conventional procedures, PMCTA offers critical advantages in criminal investigations.
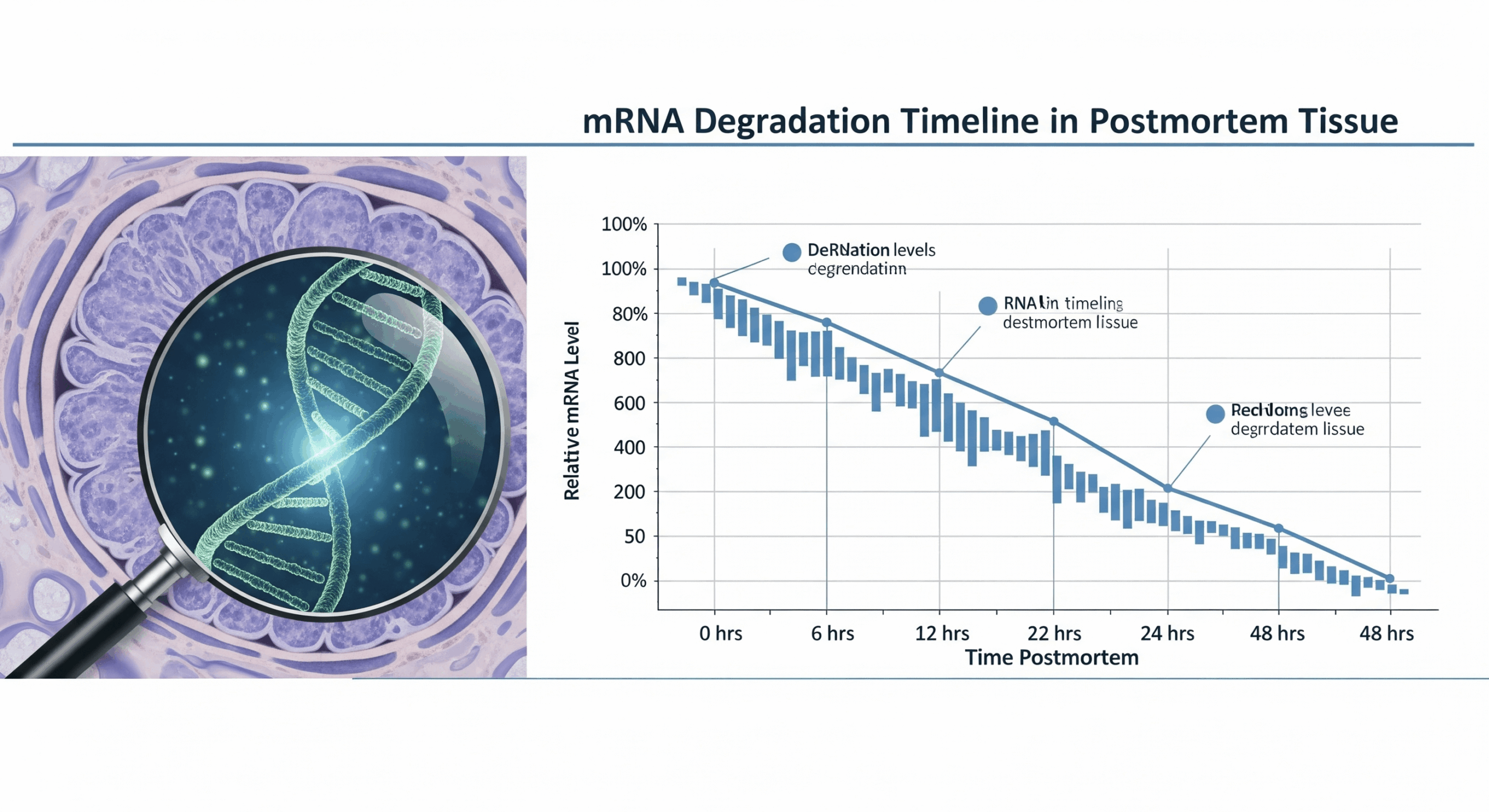
Magnetic Resonance Spectroscopy for Time of Death Estimation
Determining when death occurred remains one of forensic science’s most persistent challenges. Magnetic resonance spectroscopy (MRS) addresses this problem through biochemical analysis rather than traditional physical measurements.
Research demonstrates that 31P magnetic resonance spectroscopy can estimate post-mortem intervalThe post-mortem interval (PMI) is the time that has elapsed since an individual's death. When the time of death is not known, the interval may be estimated, and so an estimated time of death is established. Read Full Definition (PMI) by measuring the ratio of ATP to inorganic phosphate, showing a predictable exponential decrease up to 8 hours after death. Studies have tracked this ratio falling from 0.445 to 0.032 during the first 24 hours post-mortem, allowing investigators to calculate PMI with 95% confidence using inverse logarithmic functions.
Unlike conventional time-of-death estimation relying on body temperature, MRS focuses on metabolic changes less influenced by environmental factors. Recent studies have identified six key metabolitesA metabolite is a compound produced due to metabolic processes or metabolic reactions within an organism. Metabolism refers to the collective chemical processes that occur within living cells to maintain life, including energy production, growth, Read Full Definition showing strong positive linear correlation with PMI: hypoxanthine, choline, creatine, betaine, glutamate, and glycine. Samples from vitreous humor (eye fluid) yield the most consistent results, likely because this fluid’s higher viscosity and isolation from blood circulation promote more uniform biochemical changes.
Microtomography for Microscopic Injury Analysis
What happens when conventional imaging cannot resolve microscopic details crucial to a case? Microcomputed tomography (micro-CT) bridges this gap by offering non-destructive imaging with micrometer-level resolution—up to 100 times sharper than medical-grade CT [14]. This breakthrough allows forensic experts to examine minute injuries and structures that would remain invisible to standard imaging techniques.
Micro-CT has proven valuable across numerous forensic applications:
- Skeletal trauma analysis – Detecting thin fracture lines in hyoid bones and thyroid cartilage in strangulation cases
- Forensic ballistics

- Tool mark analysis – Identifying characteristic marks left by specific weapons like knives and saws
- 3D evidence preservation – Creating detailed models with sub-millimeter accuracy for courtroom presentation
Perhaps most importantly, micro-CT provides information complementary to traditional histology without damaging critical evidence. ValidationValidation, often referred to as method validation, is a crucial process in the laboratory when introducing a new machine, technology, or analytical technique. It involves a series of systematic steps and assessments to ensure that Read Full Definition studies comparing micro-CT to histological examination have found a strong correlation between the methods, with micro-CT correctly identifying most skeletal injuries. Notably, micro-CT detected additional trauma features missed during initial histological analysis, highlighting its value as a supplementary tool in complex forensic investigations.
Through these specialized technologies, we can see how virtual autopsy continues to evolve, addressing previous limitations while maintaining its fundamental advantage of non-invasive examination. The integration of these advanced imaging methods enables forensic pathologists to uncover critical evidence that might otherwise remain hidden, even to the most skilled traditional autopsy practitioner.
Forensic Applications of Virtual Autopsy

Image Source: https://pexels.com/
The forensic community has embraced virtual autopsy techniques as essential tools that extend our investigative capabilities beyond traditional methods. These non-invasive digital approaches address several long-standing challenges in post-mortem examination while opening new possibilities for evidence discovery and analysis. Let’s examine how these technologies are changing real-world forensic investigations.
Trauma Pattern Analysis and Weapon Identification
When examining complex trauma patterns, PMCT demonstrates particular strengths, especially in cases involving blunt force injuries from traffic accidents, falls, or violent assaults. The ability to create 3D reconstructions of fracture patterns helps forensic experts understand fragment relationships and injury mechanisms with remarkable clarity. This capability makes virtual autopsy particularly valuable for reconstructing traumatic incidents in three-dimensional space.
Cases involving weapon identification have been significantly enhanced through this technology. In one notable investigation, forensic scientists used 3D photogrammetry to successfully match perpetrators’ shoes with imprints discovered on a victim’s face and body. For firearms investigations, PMCT offers distinct advantages—not only pinpointing bullet locations precisely but also providing critical information about their characteristics (single bullet, pellets, or fragments) and trajectory through the body [16].
Foreign Object Detection and Localization
Foreign body detection represents one of the most fundamental applications of forensic radiology. CT scanning excels here, depicting potential foreign objects three-dimensionally in a single examination, which greatly simplifies extraction planning. The technology offers another key advantage: radiodensity measurements in Hounsfield units (HU) enable precise determination of material composition, particularly valuable when examining explosion victims with multiple embedded fragments.
The accuracy rates are impressive. Research has shown that multidetector CT achieved 100% accuracy in metallic fragment localization. In general practice, PMCT consistently outperforms traditional autopsy methods in detecting and precisely locating projectiles, providing investigators with crucial information before any invasive procedures begin.
Cause of Death Determination Accuracy
How effective is virtual autopsy at determining the cause of death? Studies reveal variable accuracy depending on case type. Research shows 84% accuracy for traumatic deaths, with 82% sensitivityIn the context of laboratory equipment or analytical techniques, the term "sensitive" describes the capability of a machine or method to detect even very small amounts or concentrations of a substance. Sensitivity is a quantitative Read Full Definition and 86% specificityIn the context of laboratory equipment or analytical techniques, the term "specific" describes the capability of a machine or method to accurately and selectively detect particular molecules or substances while minimizing interference from others. Specificity Read Full Definition. However, these rates drop significantly for natural deaths where soft tissue pathologies play a more prominent role.
A comprehensive review of virtual autopsy applications found that in 65% of cases (15/23), the cause of death determined through virtual means matched the diagnosis established after traditional autopsy. PMCT provided fast and accurate injury identification in trauma patients, with 64.7% having a single definitive cause of death identified.
Disaster Victim Identification Protocols
The management of mass fatality incidents represents a particularly challenging area where virtual autopsy has proven invaluable. INTERPOL’s DVI protocols include four essential phases: scene examination, post-mortem data collection, ante-mortem data gathering, and reconciliation. Virtual autopsy technologies significantly enhance the post-mortem phase of this process.
CT scanning has demonstrated exceptional value in DVI operations by rapidly documenting dental characteristics through virtual reconstructions. While fingerprintsFingerprint, impression made by the papillary ridges on the ends of the fingers and thumbs. Fingerprints afford an infallible means of personal identification, because the ridge arrangement on every finger of every human being is Read Full Definition, odontology, and DNA profiling
The implementation of virtual autopsy techniques within standardized DVI protocols has markedly improved post-mortem investigations, especially in mass fatality incidents where time and resources are often severely limited. This application demonstrates how digital approaches can address practical challenges while maintaining scientific rigor.
Comparing Virtual Autopsy to Traditional Methods
The digital revolution in forensic medicine brings us to a critical question: How do virtual autopsies compare with traditional methods? When we examine both approaches side by side, several key differences emerge—each with significant implications for forensic practice. These differences highlight the technological advancements and the fundamental tradeoffs involved in choosing between these methodologies.
Diagnostic Accuracy Rates in Different Scenarios
The truth about virtual autopsy accuracy follows what forensic scientists call the “trauma advantage”—these digital techniques shine brightest in certain case types while struggling in others. For traumatic deaths, virtual autopsy demonstrates impressive results with 84% accuracy, 82% sensitivity, and 86% specificity. However, the picture changes dramatically with natural deaths, where soft tissue pathologies often determine the cause of death. Overall diagnostic sensitivity reaches only 67.33% compared to classic autopsy, though specificity remains remarkably high at 98.37%.
CT scanning shows particular strengths in specific scenarios. The technology proves superior when identifying complex fracture patterns, mapping bullet trajectories, and locating foreign objects. The weakness is apparent in cardiovascular investigations, where virtual autopsy without contrast enhancement demonstrates limited accuracy—sensitivity hovers around 60%. This pattern of strengths and limitations explains why, despite claims that virtual autopsy can determine the cause of death in 98% of cases, independent validation studies consistently report more modest outcomes.
Time and Resource Requirements
The efficiency advantage of virtual autopsy cannot be overstated. While traditional autopsies typically require several hours of meticulous dissection and examination, CT scanning can be completed in a mere 20 seconds to 5 minutes. This dramatic time difference translates to real-world capacityThe amount of finished product that could be produced, either in one batch or over a defined period of time, and given a set list of variables. Read Full Definition improvements. Consider the New Mexico Office of the Medical Investigator, which decreased full autopsies by 10% over five years after implementing post-mortem CT scanning—despite handling 15% more cases overall during that period.
The financial equation presents a more complex picture. The initial equipment investment creates a significant hurdle—an Anatomage virtual autopsy table alone costs approximately $60,000. Yet the long-term math may favor virtual approaches, as they typically require fewer staff members per examination. This staffing efficiency could potentially offset initial costs over time, particularly in high-volume facilities.
Preservation of Evidence
Virtual autopsy’s evidence preservation capabilities represent perhaps its most compelling advantage. Unlike traditional methods that necessarily disrupt bodily integrity, virtual examination leaves the deceased completely intact. This noninvasive approach prevents potential evidence contaminationContamination - The unwanted transfer of material from another source to a piece of physical evidence. The inadvertent touching of a weapon, thereby adding fingerprints to it is an example of evidence contamination. Read Full Definition or destruction, a critical consideration in criminal investigations.
Digital documentation adds another dimension to evidence preservation. Virtual autopsies create permanent 3D models that remain accessible indefinitely without degradation over time. Furthermore, these examinations capture information from areas not routinely examined during conventional procedures, including facial structures, the spine, and limbs. This comprehensive documentation can prove invaluable when new questions arise in ongoing investigations.
Limitations in Physiological Assessment
The digital-tactile divide marks virtual autopsy’s most significant limitation. Traditional autopsy allows examiners to assess texture, color, and smell—sensory inputs that often reveal subtle pathological changes. This tactile advantage means certain conditions, including microvascular thrombi, small tumors, and infections, remain difficult to detect through imaging alone.
Another persistent challenge involves the “post-mortem paradox”—difficulty differentiating between regular post-mortem changes and actual pathologies. For example, fluid accumulation that naturally occurs after death might be misinterpreted as bleeding, while post-mortem gases could be mistaken for air embolism. Often clear to an experienced pathologist during physical examination, these distinctions can confound even advanced imaging analysis.
Comparison with traditional autopsy
| Aspect | Virtual Autopsy | Traditional Autopsy |
|---|---|---|
| Invasiveness | Non-invasive | Invasive |
| Time | Faster (hours) | Longer (days) |
| Preservation | Maintains body integrity | Alters body |
| Cultural sensitivity | More acceptable | May conflict with beliefs |
| Data storage | Digital, easily shareable | Physical, limited access |
| Radiation exposure | Minimal | None |
Technical Challenges and Scientific Limitations
Despite virtual autopsy’s promising capabilities, several significant technological hurdles limit its widespread implementation in forensic medicine. These challenges represent critical barriers that must be overcome before digital post-mortem analysis can reach its full potential.
Current Hardware Constraints
The financial barrier to entry presents perhaps the most formidable obstacle. Initial construction costs for dedicated virtual autopsy laboratories range from 3 to 5 million RMB, with annual maintenance expenses adding approximately 30,000 RMB. What specific equipment limitations do forensic facilities face? Three primary issues emerge:
- Standard CT scanners with 3.5 MHU tubes commonly overheat during corpse scanning, substantially reducing workflow efficiency
- Higher-capacity tubes (>5.3 MHU) offer more reliable performance but at significantly greater cost
- MRI devices, while essential for comprehensive soft tissue examination, see limited implementation due to lengthy scanning times and prohibitive expenses
These hardware limitations create a two-tier system where only well-funded institutions can fully utilize virtual autopsy technologies. Meanwhile, smaller facilities must either forgo these capabilities or develop strategic partnerships with better-equipped institutions.
Software Development Needs
The software architecture supporting virtual autopsy reveals another layer of challenges. Current systems typically operate through an unwieldy combination of tracking servers (running in 32-bits) and navigation applications (compiled in 64-bits) to manage the massive CT datasets. This arrangement works but remains far from optimal.
Automatic registration capabilities, essential for streamlining workflows, continue to underperform. These systems frequently fail when foreign bodies generate false positives during marker detection. What’s needed? Enhanced algorithms that can accurately distinguish between anatomical landmarks and post-mortem artifacts. Without these improvements, technicians must perform time-consuming manual corrections, negating much of the efficiency virtual autopsy promises.
Data storage and security
The large amount of data generated by virtual autopsies presents unique challenges:
- Long-term data preservation and accessibility must be ensured for future reference
- High-capacity storage systems are needed to handle the volume of imaging data
- Robust security measures must be implemented to protect sensitive information
Legal and ethical considerations
Virtual autopsies raise several legal and ethical questions:
- Admissibility of virtual autopsy evidence in court
- Privacy concerns regarding digital storage of detailed body scans
- Cultural and religious objections to certain imaging procedures
These issues must be carefully addressed to ensure virtual autopsy technology’s ethical and legal use.
Standardization of Protocols
No universally accepted protocol currently exists for virtual autopsy procedures. This lack of standardization leads directly to inconsistent imaging interpretation across different forensic experts. The absence of large-scale validation studies further compounds this problem by hindering the establishment of reliable diagnostic criteria.
The digital nature of evidence raises additional concerns. Unlike physical specimens, digital images can be altered by changing, moving, or deleting pixels—sometimes without leaving obvious traces. Consequently, forensic communities must implement strict chain-of-custody guidelines for image processing to maintain evidence integrity. Without such protocols, courts may increasingly question the admissibility of virtual autopsy findings.
Training Requirements for Forensic Radiologists
The workforce development challenge may ultimately prove most limiting. Interpreting postmortem images demands specialized knowledge fundamentally different from clinical radiology. Normal postmortem changes frequently mimic pathological conditions—fluid seepage can appear identical to antemortem bleeding, while postmortem gases might be indistinguishable from fatal air embolism.
Virtual autopsy implementation, therefore, requires dedicated educational programs focused specifically on forensic radiological interpretation. Until these training gaps are addressed comprehensively, most institutions will continue relying on clinical imaging experts for auxiliary diagnosis. This stopgap approach creates potential diagnostic blind spots when clinicians unfamiliar with post-mortem changes misinterpret normal decomposition as pathology.
The path forward requires systematically addressing these challenges. Hardware improvements must be paired with software refinements, standardized protocols, and specialized training. By tackling these interconnected issues, we can only fully realize the promise of virtual autopsy in forensic medicine.
Future of Virtual Autopsy
Emerging trends
Virtual autopsy is rapidly evolving, with several exciting trends on the horizon:
- AI-powered analysis: Machine learning algorithms are being developed to assist in interpreting imaging data, potentially identifying patterns and anomalies that human observers might miss.
- Enhanced 3D visualization: Advanced rendering techniques are improving the clarity and detail of 3D models, allowing for more accurate virtual dissections.
- Integration of molecular imaging: Combining traditional CT and MRI scans with molecular imaging techniques like PET scans to provide more comprehensive insights into cause of death.
| Trend | Description | Potential Impact |
|---|---|---|
| AI analysis | Machine learning algorithms assist in data interpretation | Improved accuracy and efficiency |
| 3D visualization | Advanced rendering for clearer virtual dissections | Enhanced detail and precision |
| Molecular imaging | Integration of PET scans with CT/MRI | More comprehensive insights |
Potential for widespread adoption
The future of virtual autopsy looks promising, with increasing potential for widespread adoption:
- Cost-effectiveness: As technology becomes more accessible, virtual autopsies may become more economical than traditional methods.
- Cultural acceptance: Virtual autopsies offer a non-invasive alternative, potentially increasing acceptance in cultures with reservations about traditional autopsies.
- Training and education: Virtual autopsies provide excellent tools for medical education and forensic training without the need for physical cadavers.
Integration with other forensic tools
The integration of virtual autopsy with other forensic tools is set to revolutionize death investigations:
- Crime scene reconstruction: Combining virtual autopsy data with 3D crime scene scans for comprehensive case analysis.
- Toxicology integration: Linking toxicology reports directly to 3D body models to visually represent substance distribution.
- Genetic analysis correlation: Integrating genetic data with virtual autopsy findings to identify hereditary conditions or predispositions.
As these advancements continue, virtual autopsy is poised to become indispensable in forensic science
Conclusion
Virtual autopsy represents a remarkable advancement in forensic science. It combines cutting-edge imaging technologies with noninvasive examination techniques. This approach gives us unprecedented insights into post-mortem findings while preserving the body’s integrity—a significant advantage in criminal investigations and cases involving cultural or religious considerations.
What makes virtual autopsy particularly valuable in forensic medicine? Research clearly demonstrates its strengths in three key areas: trauma analysis, foreign object detection, and disaster victim identification. For traumatic deaths specifically, studies show diagnostic accuracy rates reaching 84%, though effectiveness varies significantly based on case type. The technology particularly excels at visualizing complex fracture patterns and bullet trajectories—areas where traditional methods often face limitations.
Despite these promising capabilities, substantial technical challenges remain. Hardware costs present significant barriers to adoption, while software development needs and standardization requirements create operational hurdles. Medical facilities face difficult decisions when weighing substantial initial investments against potential long-term benefits such as increased case processing efficiency and permanent digital evidence preservation.
The future of post-mortem examination likely involves a complementary approach. Virtual autopsy continues evolving, addressing previous limitations while maintaining its fundamental advantage of non-invasive analysis. This progress points toward forensic practice where digital and traditional methods work in tandem, enhancing our capacity to uncover critical evidence and serve justice effectively. As technology advances, we can expect virtual autopsy to play an increasingly vital role in modern forensic investigations.
FAQs
What are the main advantages of virtual autopsy over traditional methods?
Virtual autopsy is non-invasive, preserves bodily integrity, and creates permanent digital records. It’s faster, can handle more cases efficiently, and excels at analyzing complex trauma patterns and foreign object detection.
How accurate is virtual autopsy in determining the cause of death?
Accuracy varies depending on the type of death. For traumatic deaths, virtual autopsy shows about 84% accuracy. However, accuracy is lower for natural deaths involving soft tissue pathologies. Overall, studies indicate a diagnostic sensitivity of around 67% compared to traditional autopsy.
What technologies are used in virtual autopsy?
Virtual autopsy primarily uses computed tomography (CT) scanning, magnetic resonance imaging (MRI), and 3D surface scanning. Advanced techniques like post-mortem angiography and magnetic resonance spectroscopy are also employed for specific analyses.
Can virtual autopsy completely replace traditional autopsy methods?
While virtual autopsy has significant advantages, it cannot entirely replace traditional methods. It struggles to detect certain conditions, like small tumors and infections, and lacks the tactile information conventional autopsy provides. Ideally, both methods should be used complementarily.
What are the main challenges in implementing virtual autopsy systems?
Major challenges include high initial equipment costs, the need for specialized software development, a lack of standardized protocols, and the requirement for extensive training of forensic radiologists. Overcoming these hurdles is crucial for the widespread adoption of virtual autopsy techniques.
References & Further Readings
[1] – https://en.wikipedia.org/wiki/Virtopsy
[2] – https://pmc.ncbi.nlm.nih.gov/articles/PMC4580998/
[3] – https://www.rsna.org/news/2016/march/virtual-autopsy-connects-radiology-and-forensics
[4] – https://www.sciencedirect.com/science/article/abs/pii/S037907381200134X
[5] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10543514/
[6] – https://www.theguardian.com/science/2013/feb/23/virtual-autopsy-virtopsy-forensic-science
[7] – https://nij.ojp.gov/topics/articles/postmortem-ct-scans-can-they-effectively-replace-full-autopsies
[8] – https://pmc.ncbi.nlm.nih.gov/articles/PMC4067017/
[9] – https://www.sciencedirect.com/science/article/abs/pii/S2212478015300319
[10] – https://asomef.org.co/wp-content/uploads/2020/04/3-G8A-Practical-Guide-to-Virtual-Autopsy-Why-When-and-How.pdf
[11] – https://pmc.ncbi.nlm.nih.gov/articles/PMC5450483/
[12] – https://pubmed.ncbi.nlm.nih.gov/30686369/
[13] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10486680/
[14] – https://anatomage.com/table/
[15] – https://www.rsna.org/news/2018/may/post-mortem-ct-angiography-illuminates
[16] – https://pubmed.ncbi.nlm.nih.gov/24819799/
[17] – https://analyticalscience.wiley.com/do/10.1002/sepspec.147c5fa821b/
[18] – https://www.news-medical.net/whitepaper/20210223/NMR-can-Provide-Accurate-and-Reliable-Time-of-Death-Analysis-in-Forensic-Science.aspx
[19] – https://pubmed.ncbi.nlm.nih.gov/30769301/
[20] – https://link.springer.com/article/10.1007/s40336-022-00510-y
[21] – https://www.news-medical.net/life-sciences/Validating-Micro-CT-for-Forensic-Investigations.aspx
[22] – https://link.springer.com/article/10.1007/s00414-025-03461-x
[23] – https://pmc.ncbi.nlm.nih.gov/articles/PMC6197109/
[24] – https://journals.lww.com/jfsm/fulltext/2024/10040/current_status_of_forensic_virtual_autopsy.10.aspx
[25] – https://www.researchgate.net/publication/228100180_Weapon_identification_using_antemortem_computed_tomography_with_virtual_3D_and_rapid_prototype_modeling-A_report_in_a_case_of_blunt_force_head_injury
[26] – https://pubs.rsna.org/doi/abs/10.1148/radiol.2402050972
[27] – https://www.sciencedirect.com/science/article/pii/S2153353922003418
[28] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10184261/
[29] – https://journals.sagepub.com/doi/10.1177/00031348221078985?icid=int.sj-abstract.similar-articles.2
[30] – https://www.interpol.int/en/How-we-work/Forensics/Disaster-Victim-Identification-DVI
[31] – https://pmc.ncbi.nlm.nih.gov/articles/PMC5734849/
[32] – https://onlinelibrary.wiley.com/doi/10.1111/1556-4029.15513
[33] – https://www.researchgate.net/publication/236457720_Feasibility_and_validation_of_virtual_autopsy_for_dental_identification_using_the_Interpol_dental_codes
[34] – https://pmc.ncbi.nlm.nih.gov/articles/PMC6106125/
[35] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8629304/
[36] – https://www.mdpi.com/2077-0383/14/3/782
[37] – https://virtual-autopsy.com/faq/
[38] – https://journals.sagepub.com/doi/10.1177/09710973251327639
[39] – https://www.scientificamerican.com/article/virtues-of-the-virtual-autopsy/
[40] – https://www.linkedin.com/pulse/conventional-vs-virtual-autopsy-evolving-practices-forensic-vcbse
[41] – https://pmc.ncbi.nlm.nih.gov/articles/PMC3826044/
[42] – https://ajronline.org/doi/10.2214/AJR.13.11957
[43] – https://pmc.ncbi.nlm.nih.gov/articles/PMC11818485/
[44] – https://www.auntminnie.com/clinical-news/article/15666713/radiologists-rts-and-the-art-of-forensic-imaging